If the payer asks to add the claim filing indicator, follow the steps below. Let’s have HMO as an example.
Check the implementation guide under revenue management. Go to Activities >> Revenue Management >> Implementation Guide >> Select the last “maps” icon.
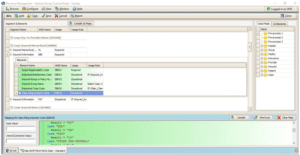
Open Loop 2000B >> Insured Information >> Claim Filing Indicator then change the Result indicator or acronym. The clearing house is the one who informs us the correct indicator. In this HMO example, it shows here “HM”.
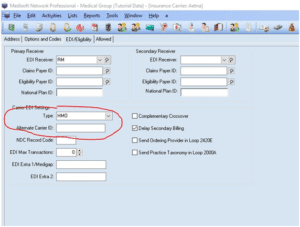
Then go to the insurance list and select which HMO insurance you are assigning this. Open EDI/Eligibibity tab then under Carrier EDI Settings type, select HMO.


Recent Comments